Blogs

To reach Medicaid members, payers are looking for a solution that will meet members where they are, resulting in effective engagement at the lowest cost.
Technology that boosts efficiency helps increase engagement and capture qualifying information, such as employment, income, and health and risk status. Payers also need help navigating members to take the appropriate action to retain their Medicaid coverage.
Share this news: LinkedIn | Twitter | Facebook
Care Angel’s simple and effective approach helps payers. Our 28% to 83% engagement rate with Angel is consistent across voice, secure chat, and text options. Payer clients should expect to increase their traditional outreach capacity by 600x or more with Angel, our digital health engagement platform.
We sat down for a Q&A with Bud Flagstad, Care Angel’s CEO, to discuss ways to boost outreach efforts during Medicaid determination.
Care Angel: What’s different about Care Angel?
Bud Flagstad: For starters, we have trained Angel for over seven years with medical and health language knowledge. That gives us context for conversations with members. It also allows us to automate repetitive, high-volume tasks. Our campaigns help us reach members; in this case, letting them know about the need to reapply for insurance coverage.
We also help payers identify care gaps quickly and efficiently. Angel can understand conversations in more than 72 languages. That helps us reach diverse populations across the country—how and when they want to be engaged.
Care Angel: What have you learned about when and how to contact members?
Flagstad: We have access to a wealth of data about members, which means we know when they’re more likely to respond and what type of outreach is more likely to generate responses. For example, Medicare members are less likely to respond during “The Price is Right,” while Medicaid members are more likely to interact at certain times using their smart phones via voice or text.
We can circle back with these members using voice, text, and secure chat. Unlike a traditional contact center employee, who may only have time to dial once, our technology can redial, which means we have a better chance of connecting with members. Our technology gives us the flexibility to start with voice and shift to other modalities based on user preferences.
Care Angel builds profiles of members, using the cognitive abilities of our AI model. While most plans have consent to text approximately 5% of their Medicaid population, we’re able to reach and gain consent for texting between 24% to 32% of their population, depending on the campaign. While complying with all appropriate regulations, Angel can engage with members using voice, text, and secure chat whenever they’re most likely to be available.
Staffing nurses at a call center after business hours is virtually impossible, but Angel provides the ability to engage with members—and that means we’re connecting when members are available.
Care Angel: But a payer executive may already have the budgeted dollars to staff a call center. What then?
Flagstad: Payers will save a significant amount of budget dollars by working with Care Angel—and those dollars can be used for other initiatives.
Angel captures information while providing education and navigation support for members—without adding to labor costs. Adaptable and customizable for other costly and critical engagement needs, Angel supports the following programs:
Enrolment and awareness
Maternal health and well-child
Diabetes quality measures
Chronic condition management
Medication and care plan compliance
Post-discharge/readmission avoidance
SDoH and health equity, and more
Care Angel keeps it simple. We're going to help you meet or exceed your Medicaid redetermination targets and keep your members covered.

It’s spring and we are excited about the future of the most meaningful kind of digital health yet! Virtual care has paved the way towards using technology to deliver healthcare at a distance and member adoption is soaring. In fact, according to an article in the National Law Review, at least 7 million patients in the U. S. will access telemedicine services in 2018.
Share this news: LinkedIn | Twitter | Facebook
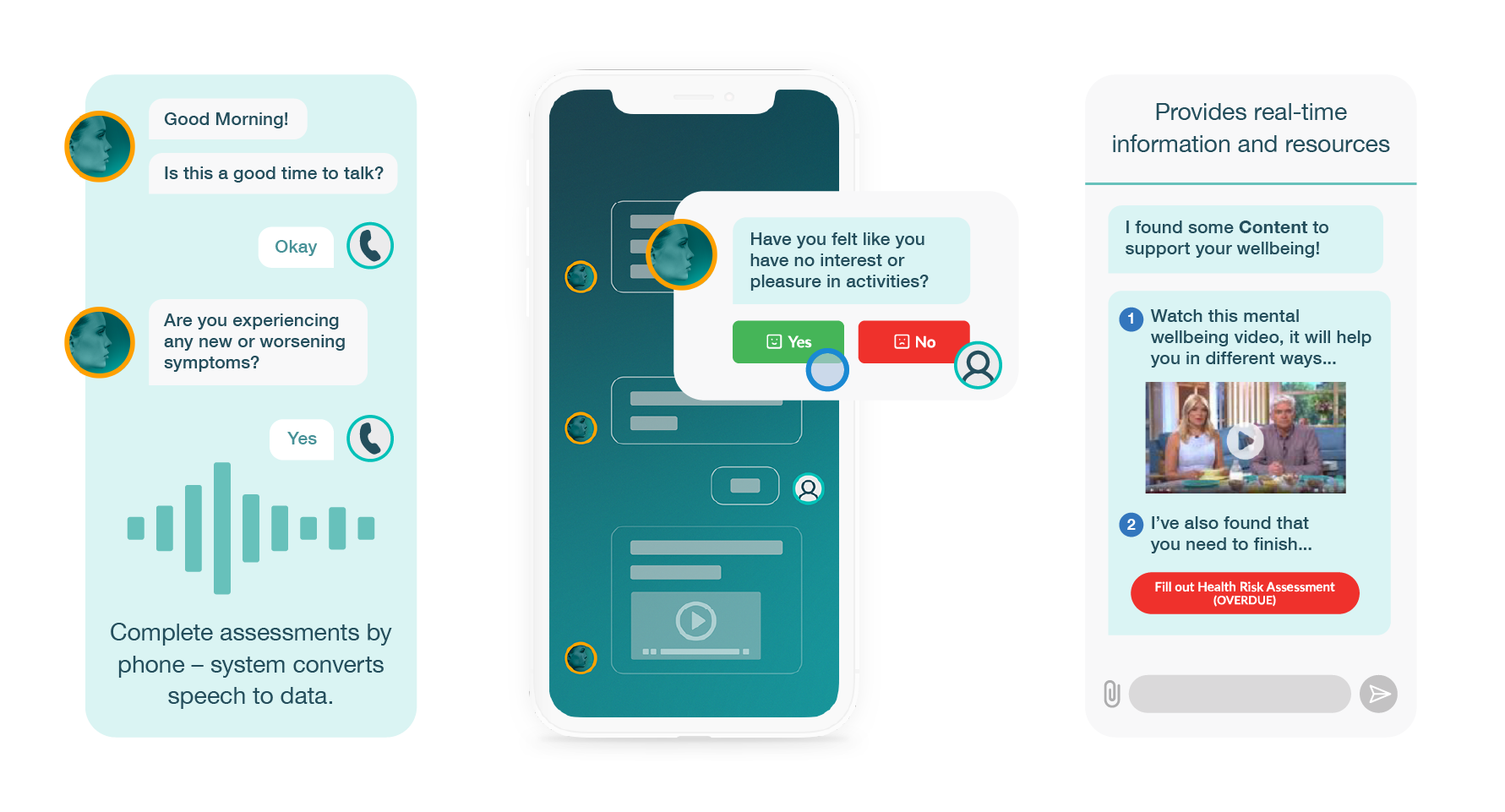
Care Angel is combining the capabilities of virtual health and artificial intelligence (AI) to expand the versatility of patient engagement to create a truly patient-centered approach to care, beyond acute episodes. Patient monitoring and health management using Angel, our intelligent, virtual nurse assistant, allows doctors, payers and their patient members to communicate bi-directionally between office visits or after hospitalization to improve care plan adherence, patient satisfaction and health outcomes.
AI is actually humanizing modern healthcare and enabling more frequent connections to effectively and efficiently close gaps in care, empowering the patient at home.
Here are 5 ways that AI is helping to redesign healthcare for
the better:
1. PATIENT CENTERED
AI and telehealth are the perfect combination for personalized health monitoring and data gathering of your patient's vitals and wellbeing to foresee potential problems before they occur. Patients are becoming more tech-savvy and want to manage their health using technology.
2. CARE PLAN AND MEDICATION ADHERENCE
Comprehensive care that proactively manages chronic conditions automatically. Keeps medication adherence and care coordination in check for tens of thousands of patients. Custom workflows, including live transfers to provider helps to drive the highest quality and efficiency at the lowest cost for all stakeholders.
3. CLINICALLY EFFICIENT
Imagine if each nurse or care manager could be 300% more efficient. AI and voice solutions allow physicians and clinicians to focus on where they create the most value; the patient encounter. Angel takes the repetitive, redundant tasks away from the caregivers, so they can practice at the top of their license.
4. REDUCE MISSED CARE OPPORTUNITIES
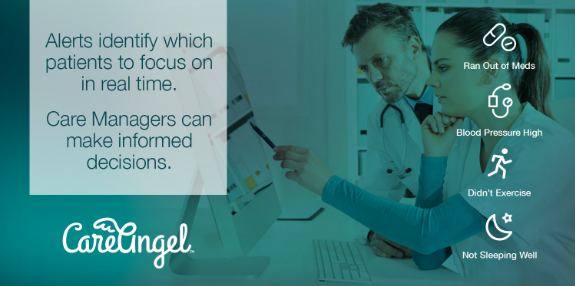
Meeting patients “at their need”, helps the patient to stay on course with treatment plans and increases provider awareness of potential gaps in care. When a medical need arises, the provider is notified in real time with the knowledge they need, leading to improved patient outcomes and better manage whole populations.
Here’s a short video that how AI and voice drives meaningful engagement:
{{ script_embed('wistia', '140wwfqni3', '', 'inline,responsive') }}
5. COST EFFECTIVE DISEASE MANAGEMENT AT SCALE
How many times have you uttered these 5 words? “If only we’d known sooner.” Knowing in advance when a patient didn’t sleep well, was in pain, had out of range vitals, was in need of medical supplies or medical services can help protect the patient from an adverse episode or hospitalization.
How do we make healthcare better and more human?
Think of it this way: The more specifically you can identify the patients that are in need and what those needs are, the more likely it is that you’ll be able to close those critical gaps in care.
Consider what would happen if you could stop spending hours and hours trying to identify patients in need of intervention? Imagine if a nurse assistant could notify you when a patient was in need of attention. In just 1-2 minutes, care managers can review the specific alert, which includes longitudinal data, and appropriately take decisive action to resolve the issue.
The game truly changes when an entire community is rallied toward solving the challenge of making healthcare more human.

When it comes to healthcare engagement, there's a myriad of ways to communicate: email, video, SMS, IVR, direct mail, telephone and the list goes on. Among all these options, voice offers the most advantages in touching lives, but until now, it just wasn't affordable to scale.
Today, there is a rapidly growing trend of AI and Voice as an interface to scale quality healthcare engagement, monitoring and management. Here's why:
Low to no barrier to entry
Easily adopted by all ages
Enables connection without the need for expensive devices or wifi service
Creates an emotional bond and has the capability to learn over time
Provides bi-directional experience that other engagement methods do not deliver
Collects data and analytics that can identify and respond to risk in real-time
CLOSE GAPS IN CARE
At Care Angel we understand that the entire healthcare experience revolves around the patient. From that core premise, we see countless examples among our healthcare partners successfully achieving condition-specific, voice-first, patient engagement that results in:
Extending care beyond the clinical setting into the home, regularly and continuously
Identifying patients who are in need of care, avoiding missed care opportunities
Improving triage, intervention and the delivery of remote care when deemed necessary
Empowering the patient and their family caregivers by giving them the tools and voice to participate in their own health, wellbeing and care plans
Reducing clinical and operational costs, improving ROI and patient satisfaction
LET’S LOOK AT THE DATA
17% is the average avoidable hospital admission (caused by gaps in care)
22% is the average avoidable hospital readmission (caused by gaps in care)
$10-25K is the average cost for a Medicaid patient readmission
At Care Angel, we align actionable data and advanced analytics so that providers and care teams, like you, can better care for populations. Together, we have reduced avoidable readmissions by 63% and lowered clinical costs by over $496k, per one thousand patients, annually.
THESE 5 STEPS GUARANTEE YOUR SUCCESS
Step 1: Personalized welcome call to the patient, from the familiar voice of their provider to build rapport and reinforce engagement
Step 2: Proactive Care Calls across entire populations. Consistent, evidence-based care plans based on chronic condition(s)
Step 3: Automatically trigger alerts that identify patients needing attention, in real-time to help care teams avoid missed care opportunities
Step 4: One click live transfers to seamlessly connect to clinician or care team for triage or intervention and resolution
Step 5: Real-time data and analytics, plus quarterly contract performance reporting, including avoidable hospital admission and readmission reduction and improved outcomes
Organizations such as payers, providers, MCO’s, ACO’s, MSO’s, IPA’s and others that manage costly, high-risk Medicare and Medicaid populations can achieve the highest health engagement, monitoring and management in the industry by using Angel, Virtual Nurse Assistant.
We place the patient at the center of the eco-system to deliver a level of engagement that has never before been possible.
AI and Voice is a trend we are seeing on the rise for 2018 as evidenced by these papers and articles recently published:

With seasonal changes often come thoughts of personal and professional improvement—how can I approach this new time of year in a way that allows me to lead a better, healthier life? Now that summer is fading and fall is fast approaching there is arguably no better time to appreciate the impact of change, particularly in regards to how you can help improve the health of your members and patients.
Share this news: LinkedIn | Twitter | Facebook
In recent years AI (artificial intelligence) has blossomed as a leading source of improving healthcare engagement, management, monitoring and care coordination. The development of technology has paved the way for a multitude of remote care delivery options to continuously care for those with one or more chronic conditions. There is solid proof that the nation has embraced the change to digital health tremendously; in fact, with each passing season, utilization of virtual care is soaring. According to an article in the National Law Review, at least 7 million patients in the U. S. will access telemedicine services in 2018.
Care Angel is combining the capabilities of virtual health and AI with voice to expand the versatility of patient engagement, creating a truly patient-centered approach to care beyond acute episodes. By means of our intelligent virtual nurse assistant, Care Angel has developed an exceptional approach to patient monitoring and health management that is a game-changer. Our AI enabled virtual nurse assistant, Angel allows providers, payers, members, and patients to communicate bi-directionally between office visits or after hospitalization to improve care plan adherence, patient satisfaction, health and financial outcomes.
AI is actually humanizing modern healthcare and enabling more frequent connections to effectively and efficiently close gaps in care, empowering the patient at home. Here are 5 ways that AI in healthcare is improving whole-patient health management for the better:
#1 Patient Centered
Automated Intelligence (AI) and voice are the perfect combination for personalized health monitoring and data gathering when it comes to your patient's vitals and wellbeing. Our real-time alerting system allows you to foresee potential problems before they occur. Additionally, patients are becoming more tech-savvy and want to manage their health using technology; Virtual nurse assistants deliver the perfect outlet for that desired interaction without the barriers of complicated devices or expensive hardware.
#2 Care Plan and Medication Adherence
Virtual nurse assistants comprehensively and proactively promote chronic condition management on a consistent basis. This keeps medication adherence and care coordination in check for tens of thousands of patients. Our HIPAA compliant platform also feeds into custom workflows (including live transfers to providers or call centers) to help drive the highest quality and efficiency at the lowest cost for all stakeholders.
#3 Clinically Efficient
Imagine if each nurse or care manager could be 300% more efficient. Virtual nurse assistant, voice solutions allow physicians and clinicians to focus on where they create the most value: the patient encounter. Automated intelligence takes the repetitive, redundant tasks away from the caregivers so they can practice at the top of their license capabilities.
#4 Reduce Missed Care Opportunities
Meeting patients “at their need” helps the patients stay on course with treatment plans and increases provider awareness of potential gaps in care. When a medical need arises, the provider is notified in real time with the knowledge he or she needs, leading to improved patient outcomes and better healthcare management over greater populations.
Check out this short video that explains how our virtual nurse assistant, Angel, comes to life to drive meaningful engagement and effectively, efficiently manage populations at scale:
#5 Cost Effective Disease Management at Scale
How many times have the following 5 words been used in reference to a healthcare management experience? “If only we’d known sooner.” Knowing in advance when a patient didn’t sleep well, was in pain, had out of range vitals, was in need of medical supplies or medical services can help protect the patient from an adverse episode or hospitalization.
How Do We Make Healthcare Better and More Human?
Ironically, with changing, advancing AI technology has come the ability to change and advance the humanistic approach to healthcare management. Think of it this way: the more specifically you can identify the patients that are in need and what those needs are, the more likely it is that you’ll be able to close those critical gaps in care. This will not only lead to an excellent patient experience, it will also allow for an efficient use of provider time and resources.
The game truly changes when an entire community is rallied toward solving the challenge of making healthcare more human. Interested in learning more? Contact Care Angel today and begin your journey toward better healthcare management with our virtual nurse assistant, Angel.
When it comes to navigating the care for high-risk, vulnerable patients or loved ones, constant monitoring and engagement is required of healthcare providers and family members in order to maintain positive patient health outcomes. Care Angel is using artificial intelligence to rewrite healthcare management strategies through the use of Angel: the world’s first virtual nurse assistant.
Share this news: LinkedIn | Twitter | Facebook
Care Angel’s voice powered virtual nurse assistant can help ease daily population health management for payers and providers that are taking risk and responsibility for patient health outcomes. This innovative virtual nurse assistant leverages real-time clinical and non-clinical data and analytics to confidently make informed decisions that prevent unnecessary ED visits and readmissions.
Whether you’re managing the efficiency and effectiveness of patient access and care delivery centered around chronic condition management, or want to close gaps in care post-discharge, the way forward is AI-powered technology. Specically, AI-driven technology that knows who is doing well and who is not in real time.
Meet Angel: The 24/7 Listening and Learning Virtual Nurse Assistant
How does Angel work? Angel extends beyond episodic care, and serves to address everyday health and chronic care management. Through personalized calls, alerts, and notifications to clinicians, and optional connectivity to family caregivers, Angel provides peace of mind without sacrificing high-quality care. This first-of-its-kind virtual nurse assistant utilizes robust data and analytics to ensure better results, and provides benefits in terms of engagement solutions, chronic condition monitoring, and healthcare management platforms.
Engagement Solution
Enables smart and dynamic technology that helps with care plan and medication adherence
Provides personalized, guided conversations by voice, reducing technology barriers
Allows for continuous, proactive engagement and care coordination between visits
Collects biometrics and other useful data regarding patient wellbeing automatically
Informs clinical decision support in real time
Resolves issues before a negative episode or hospitalization occurs
Chronic Condition Monitoring
Offers best in class, out-of-the box, evidence-based care plan templates
Evolves conversational automatically over time as patient needs change
Listens for indicators that could result in adverse outcomes for patients and members
Provides care between visits to most vulnerable, at-risk care recipients
Healthcare Management Platform
Not limited to one set of functions, rules, logic, or script
Allows the provider or payer to set the frequency of care “touches”
Makes data actionable the minute it’s received (Legacy systems can only store data)
Offers optional functionality to enable families to help reinforce care
Empowers the patient to adopt healthy behavior choices using omni-channel conversations
Want to Learn More? Get in Touch with EmpowerHealth Today!
Our virtual nurse assistant can benefit health systems, health plans and insurers, caregivers and families, and of course, care recipients. Let’s begin a conversation. Contact us today by calling (800) 825-3227 or filling out our online form!

The trend of “aging in place” is steering the care management industry in a new direction. Care Angel is proud to offer a simple yet effective, innovative breakthrough the remedy pain points in this system. Our AI-driven form of healthcare management is world-class solution, which closes the gaps in care that result in hundreds of millions of wasted dollars every year. Through an artificial intelligence-powered platform, we utilize voice-first conversations to provide a customizable suite of services that redefine how we help ACOs to better manage and monitor all things related to the health and wellbeing of their members and patients.
Share this news: LinkedIn | Twitter | Facebook
Commercial or Medicare ACOs Carrying Risk for Populations Will Reap the Benefits of Care Angel
The premise of Accountable Care Organizations (ACO) is for different entities to jointly commit to the health of the patients in order to qualify for financial incentives by achieving quality and costs goals. These incentives have stimulated more patient engagement, monitoring, and preventive care in order to reduce emergency room visits and readmissions that drive up costs. According to 2017 CMS performance data, 60% of ACOs saved money in 2017 and 34% of ACOs earned shared savings.
At Care Angel, we believe that to successfully manage the health of these Medicare populations, ACOs must monitor at a more granular level to proactively triage and treat patients in ways that will result in better health outcomes and greater shared savings.
How Does Care Angel Support ACO Partners?
Effective ACOs must share the same level of commitment to collaborating and sharing information in order to bridge gaps within patient care. Each provider must work to seamlessly communicate with patients’ and other providers to ensure that the quality of care is optimal, in order to meet the requirements for financial rewards, bonuses, and other shared savings. ACOs must also successfully rely on the data provided through digital check-ins that monitor vitals, wellbeing, and medication adherence to ultimately accomplish the goals of the ACO to reduce unnecessary emergency department visits and improve clinical outcomes.
Simply put, Care Angel removes barriers that limit timely access. Angel supports the necessary collaborative mindset that is tantamount to population health and provides real-time data and analytics that can be assessed by all stakeholders, including the patients and their family caregivers.
Why Choose Care Angel for your Innovative Population Health Solution?
A partnership with Care Angel guarantees a reduction in inefficiency and waste, and addresses a whole host of other common challenges faced by health systems, providers, and insurers, like:
Inefficient use of clinician time and skills
Ineffective method of identifying risk
High administrative cost and operational complexity
Decreased care team efficiency and effectiveness
Poor outcomes, resulting in readmission
It’s estimated that more than 1/3 of the nation’s $3.2 trillion healthcare spending is wasteful. Care Angel helps to eliminate waste as well as:
Increase provider and care team capacity
Identify patients who need care in real time
Notify in real-time and enables live transfers
Maximize clinical efficiency and effectiveness
Lower costs and improves productivity
Improve financial, clinical outcomes and industry benchmarks
Get the Benefits of Care Angel’s, Innovative AI-Driven Healthcare Management
At Care Angel, we’ve made it our mission to accomplish all of the above benefits for healthcare. We are committed to serving ACOs in a personalized way through a wide range of innovative services that meet each individual client’s needs. Angel, our virtual nurse assistant, propels the advancement of healthcare management forward through innovative AI technology, while keeping the human touch central to the equation. If you want to explore the most effective ways to extend care and empower care teams, individuals and their families, at the lowest cost, we encourage you to take the first step and contact us today. We’ll help you get started and guide your progress every step of the way.

Care Angel CEO Wolf Shlagman Talks About AI and Virtual Nurse Assistant, Angel.
Care Angel, the brainchild of Wolf Shlagman, CEO, Founder and Chief Angel is featured in the latest publication of Insightscare 10 Most Innovative Companies Bringing AI to Healthcare
The age of the AI nurse assistants in healthcare is here. Consider that worldwide, the population who are aged 60 years or over were numbered at 962 million individuals in 2017. The case for improved automation, productivity and operational efficiency is clear.
Healthcare organizations from MSO, ACO, health systems, payers, telehealth providers, pharmacy and care management and monitoring companies are all seeking ways to improve both management and coordination of care, plus reduce costs and improve outcomes. Check out the article to see how we do it with a dynamic, omni-channel workflow that results in the highest engagement possible.
Our partner clients and the individuals they serve are able to make healthcare more human, more accessible and more proactive, resulting in a reduction of avoidable ED visits, admissions and readmissions.
{{cta('ce2c73a7-351a-4d03-8809-1851d9563652')}}


Care Angel’s award-winning, end-to-end, healthcare engagement platform is revolutionizing population health at scale - and the results are impressive.
Unlike other automated health engagement technologies, our virtual nurse assistant provides an empathetic, human touch to offer continuous and customizable health monitoring and management, at scale.
This transformational healthcare solution can:
Communicate through multi-channel modalities (EX: phone, chat, text, web, app, email, IoT)
Stratify entire populations based on risk
Manage and monitor clinical and non-clinical information
Identify and address SDoH factors that could prevent access to care
Coordinate care and scheduling tools and services
Identify and address gaps in care
Align and navigate to the right resources
Close gaps in care at exactly the right time with real-time intervention capabilities
Follow up and validate resolution
Optimize STARs/HEDIS® performance measures, generating additional revenue opportunities
From doctors and care providers to patients, partners, payers, and everyone in between, we are elevating healthcare management in ways that were previously not possible.
Most Efficient and Effective: Virtual Nurse Assistant
Care Angel stands apart from competitors by using the most natural user interface, voice. Angel becomes easily integrated into user’s life, like a family member. Angel helps to continuously manage care, checking in on individuals about vitals, pain, mood, sleep, nutrition and more - and she detects, based on responses, when a member needs additional resources like the doctor, nurse helpline, pharmacy, family caregiver or other community resource. Paired with a strong commitment to clinical quality and user design, these care calls are dynamic and personal based on the needs of the member and provide real-time alerts and notifications to designated care teams and family members. The information and data that's collected is stored in a secure, HIPAA-compliant dashboard. Angel helps connect members to appropriate resources, services, educational material or family care circle, reducing the chance of an acute episode, hospital admission, or readmission.
In the world of value-based care, it is the quality, efficiency and effectiveness of care that helps to improve outcomes and member satisfaction. While other health engagement competitors offer a chat-bot, via text, only Care Angel deploys a multi-modal approach, starting with a simple phone call. The ubiquity of the telephone can effectively communicate with 100% of populations, including seniors who are often the hardest-to-reach demographic. In many cases, patients 65+ don’t have app or smartphone capabilities, and if they do, are hesitant to use them due to lack of familiarity. Our virtual nurse assistant extends digital healthcare to everyone, requires no app download, and easily relays information directly from the patient to care teams and family. This allows continuous, proactive engagement with members that creates a longitudinal record across entire populations.
Close Gaps in Care: Outstanding Population Health Model
Our technology transforms clinical and SDoH patient data into real-time actionable interventions, resulting in lower costs, more revenue generating opportunities, improved STARs and HEDIS performance and higher patient satisfaction for payers and providers.
We help bridge gaps in care. We drive proven financial savings for health plans, mitigating risk for the costliest populations. We enhance the consumer experience for digital therapeutics pharmacy, pharma, clinical trials, PERs and other partners, supporting patient needs for communication and education around care. And we give family caregivers peace of mind with notifications about their loved-one via integrated mobile and web applications that securely organize patient responses into data to provide regular summaries of health status and trigger alerts if needs or risk is found.
Value-Based Programs: Enhance Care and Improve Outcomes
It’s easy to see why Care Angel stands out as the most robust, intelligent, and comprehensive AI and voice enabled healthcare platform. Despite the number of healthcare apps that exist, few are successful over time, that is why we believe that the best of technology must intersect with human-ness in order for innovation to become historic. Leveraging technology to enhance human connection is in the foundation of everything we do. If you’re ready to see how Care Angel’s SmartCare platform can revolutionize population management for you, take the first step and contact us. We can’t wait to show you how our virtual nurse assistant changes lives. Just ask one of our members, Rosanne!
Care Angel provides solutions for everyone from payers providers, pharma to loved ones and caregivers. The results and outcomes speak for themselves; our virtual nurse assistant is a vital tool for making care management scalable while more productive and cost efficient. Effectively touching patients exactly when intervention is needed. Contact us to learn how we can serve you and your business strategy today!
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA)
{{cta('1132796a-0131-46e1-a95d-949e7e5496a9')}} {{cta('7c9790ee-059c-4190-b10c-1cba67f79bed')}}


Managing high-risk populations like Medicare and Medicaid patients is hard and time consuming. At a time when clinical resources are scarce, Care Angel makes effective care easier with an innovative, digital health engagement service.
By identifying risk across massive populations, clients are able to proactively address and close gaps early - outside of the clinical setting.
Work Force Shortages and Care Access
Health plans and providers are facing mounting complexities. They need to address fragmented care, compliance to care plans, medication adherence, aging and polychronic populations and a major shortage of clinicians that could benefit from an augmented staff to extend outreach.
Good news: Care Angel’s impact on the overwhelmed, traditional care management models is proven to yield a 7x labor equivalency. Proactively capturing vitals, well-being and SDoH information using voice, text and chat conversations helps predict and prevent negative downstream healthcare events that lead to ED visit or (re)admission.
70% of Healthcare Costs are Preventable
The unified goal is to provide better options for managing populations, especially high risk. We can efficiently augment expensive care management, which improves care access and triage to the right resources at the right time automatically.
This powerful combination delivers:
Enhanced quality of care that improves population outcomes for both patients, providers and payers
Optimization of existing resources, enhancing clinician experience
Improved health monitoring and member engagement
More comprehensive care for broad array of conditions among high-acuity patients with diabetes, hypertension, kidney failure and high-risk pregnancy
Finding gaps and automating documentation (boosts outcomes, ROI and revenue)
What is the Most Valuable Technology for Healthcare Systems?
Augmented Intelligence, distributed through omni-channel interactions, is poised to lead the transformation of care management. Using cognitive technology to go beyond passive remote monitoring, Care Angel is already lowering labor costs, improving efficiencies, and enabling effective interactions that engage patients in a personalized way when and where they want it.to proactively identify individuals that need healthcare support.
The time for a new approach is right now. Care Angel’s virtual nurse assistant offers a new way for healthcare stakeholders to provide care needed by millions of patients, while improving outcomes.
We all know that patient health issues only get worse without effective management, meaningful engagement and timely action. Especially for chronic illnesses that require expensive care, even small changes in patient health behavior can result in better outcomes and a dramatic impact on overall healthcare costs!
Interested in trying Care Angel? Contact us today!


Burnout among healthcare workers has reached what the National Academy of Medicine called “crisis levels.” According to the nonprofit that advises the nation on issues of health, healthcare, and biomedical science and technology, 35% to 54% of nurses and physicians were reporting symptoms of burnout. And that was before the COVID-19 pandemic.
Share this news: LinkedIn | Twitter | Facebook
With its troubling impact on patient care and safety, burnout among nurses is leading many to leave the profession. A November 2021 survey by Hospital IQ found that 90% of registered nurses are thinking about leaving nursing within a year.
In addition, half a million registered nurses are expected to retire by the end of 2022; that reality led the U.S. Bureau of Labor Statistics to project that the country will need 1.1 million new registered nurses. These changes come with a steep $9 billion annual price tag, according to a recent advisory from the U.S. Surgeon General that seeks to address clinician burnout.
Sandra Hernández, president and CEO of the California Health Care Foundation, calls for healthcare organizations to address the workforce problem by taking a “major technology leap forward.” Hernández writes: “Technology is the great extender. It is the bridge between people who make up the workforce. It can bring out the best in individuals, in teams, and different systems.”
Meet Angel: Award Winning A. I. Voice Nurse Assistant
Care Angel can help defeat burnout by helping nurses work at the top of their licenses. The results are improved patient care and expanded nurse capacity. Angel does this for 15% of the cost–or even less. That’s important because healthcare organizations simply don’t have the numbers of employed nurses to make these calls to members and patients on a 1-on-1 basis.
Angel reduces nurse burnout by removing administrative work, such as dialing lists of patients that don't have an immediate need. That means nurses can focus on caring for patients that DO have clinical needs. The results: Nurses enjoy their work more and patients receive better care.
Angel comes to life through a secure, HITRUST-certified platform that supports healthcare organizations’ HIPAA compliance. Launching hundreds of thousands of personalized interactions with members and patients, Angel reaches millions of at-risk patients. That’s for post-discharge follow-up care, medication adherence, management of chronic conditions such as diabetes and hypertension, or any clinical outcome you’re striving to achieve.
Every single day, Care Angel can touch 90% to 100% of your at-risk populations and activate and engage 43%. That leaves your nurses to practice at the top of their licenses and exercise their clinical judgment, which can help prevent burnout. Angel is proven to extend care by 5 times, casting a wider net to help identify patients and guide them to the right resources–such as their physician or a pharmacy–in real time. Angel reduces the cost of care while lessening the burden on care management teams.
The end result: Improved population health outcomes, better chronic condition management, and happier nurses and patients.
Want to Learn More? Contact Care Angel Today!
To learn more about Angel, contact us today by calling (800) 825-3227 or filling out our online form. We look forward to working with you and providing you with the healthcare management tools you need!

Last month AHIP 2022 took Las Vegas by storm–and Care Angel’s team was there for it. We sat down with two of our team members who attended the conference to capture their observations. That’s Seth Miller, operations manager, and Bill Bowman, vice president of sales and business development.
Top of mind for health insurer executives is the need to pursue “a deeper relationship with large patient, member, and employer populations for use cases from chronic condition management to readmission reduction, behavioral health, and recovery from substance use disorder,” said Seth. Executives attending AHIP 2022 were “very responsive, in particular, to our voice-based demo for chronic condition management,” he added.
Bill noticed another theme at play at AHIP 2022: Namely, the need to address health inequities. Many of his conversations in Care Angel’s booth centered on “payers’ need to support underserved and marginalized populations,” he explained.
Ninety percent of the country's $4.1 trillion in annual healthcare costs are for people with chronic and mental health conditions, according to research. A survey of nearly 300 health system leaders conducted by consulting firm Deloitte found that addressing social needs as a part of clinical care is often “ad hoc.” In addition, the company’s survey found that “gaps remained in connecting initiatives that improve health outcomes or reduce costs.”
Without further ado, here are four highlights from Seth and Bill at AHIP 2022:
Marked interest in chronic condition management and the need to address health equity challenges.
“There was a lot of interest in chronic conditions, specifically diabetes, hypertension, and kidney disease monitoring,” said Seth. “A lot of people arrived at the booth with questions about how Care Angel could help them augment their current chronic condition management efforts, such as clinical outreach operations.”
Attendees that we spoke with were really interested in the ability to improve their care management of health populations at scale, he added.
Health insurer executives arrived at AHIP 2022 searching for solutions to support underserved populations, according to Bill. “Many executives were responsive to the fact that Angel works with not only mobile devices, but also landline phones, which means the health insurer can achieve interventions wherever populations exist; it also means Angel is a good fit for members who may not have access to a smartphone or reliable internet service,” he said.
Bill also observed that health insurer executives were interested in Angel’s ability to subtly correct the misspelling of medications and to reach non-English-speaking members–who, again, are underserved–with access to Angel’s ability to speak and understand more than 72 languages. “Health insurers can’t staff clinicians who speak in all of their members’ native languages,” he explained.
Increased demand for help with medication management, medical care, and surgical protocols.
Some of the reasons members don't consistently take their medications include "My medicine makes me feel sick." or "I forgot." Often, members struggle to afford their medications. But their health insurer doesn't know that if the member isn't asked about medication adherence.
The health insurer executives Bill talked to were looking for ways to improve medication management. In particular, these decision makers were interested in learning about our deep understanding of medical care, such as wound care, and surgical protocols, he said.
Chronic wounds impact approximately 6.5 people in the United States–and it’s costly: to the tune of $25 billion annually. Combine that with a rapidly aging population and a marked increase in diabetes and obesity, and we have a crisis on our hands.
Demand for behavioral health screenings is high.
One in five U.S. adults experienced mental illness in 2020, per the National Alliance for Mental Illness. And it's worse for some individuals: One in 20 people experienced a serious mental illness, while 1 in 15 experienced both a substance use disorder and mental illness.
But there’s a projected shortage of 250,000 behavioral health professionals. which means access to support is an ongoing challenge.
“Angel can help health insurers by assessing members’ upward or downward spirals and connect them with a reliable, trusted resource–such as a therapist or even a psychiatric nurse, in real time, during an acute event,” said Bill.
This same workflow offered by Angel is also a good fit for health insurers who want to “triage for situations that come up, such as high blood sugar or high blood pressure. Angel relies on machine learning to flag these events and support connections with the appropriate clinicians,” he added.
Increased interest in integrations with Care Angel
Seth was thrilled to field “a lot of questions about integrations with other software platforms,” he said.
Care Angel integrates with a wide variety of health IT platforms. We’re ready to roll up our sleeves and collaborate during design sessions to exceed your integration expectations–and make each customized, launch a quick, painless, and process-driven. Deployments are typically less than 30 days.
Meet Angel: Award Winning A. I. Voice Nurse Assistant
Every single day, Angel can touch 90% to 100% of health insurers’ at-risk populations and activate and engage 43%.
Angel comes to life through a secure, HITRUST-certified platform that supports healthcare organizations’ HIPAA compliance. Launching hundreds of thousands of personalized interactions with members, Angel reaches millions of at-risk members. That’s for post-discharge follow-up care, medication adherence, management of chronic conditions such as diabetes and hypertension, or any clinical outcome you’re striving to achieve.
South Florida-based EliteHealth, a Care Angel client, saved time, money, and resources--while increasing member engagement--from day one. Here are three ways EliteHealth achieved these goals:
83% increased member engagement as a result of interactions with Angel that are intelligent, personalized, conversational, and data-driven.
63% reduction in avoidable hospital readmissions as a result of real-time alerts and scale-effective interventions.
15:1 ROI, which means they can maximize clinical efficiency, lower costs, improve outcomes, while serving as good stewards of members' premium dollars and CMS' investment in beneficiaries.
The end result: Improved population health outcomes, better chronic condition management, and more effective use of resources.
Want to Learn More? Contact Care Angel Today! To learn more about Angel, write us at hello@careangel.com or fill out our online form. We look forward to working with you and providing you with the healthcare management tools you need!

Leveraging augmented intelligence via voice, text, and secure chat to bring care into the home. Healthcare organizations can massively scale patient engagement, care management and population health to proactively detect possible risk. Here are 6 reasons to look into AI nurse assistants:
1. Transformative technology with low- to no barrier to entry
2. Easily adopted by all patient populations, including seniors
3. Enables connection without expensive devices or Wi-Fi service
4. Promotes a path to whole-person health, with capability to learn over time
5. Offers a bi-directional experience that other engagement methods can't deliver
6. Collects clinical and well-being data that identifies needs and can respond to risk in real-time
Share this news: LinkedIn | Twitter | Facebook
Close Gaps in Care
Payer and provider organizations can super charge their digital engagement with high tech and high touch, achieving condition-specific, patient engagement to reduce missed care opportunities. Sophisticated scheduling rules are applied for various communication modalities to meet members how and where they want to be met.
That’s in addition to increasing clinical capacity, reducing clinical and operational costs, improving ROI, and member/patient satisfaction.
Patients and their family caregivers also seek empowering tools to participate in their own health, well-being, and care plan adherence at home.
5 Best Practices for Member and Patient Engagement
These 5 steps guarantee payer, provider and value-based care organizations’ success:
Step 1: Introduce patients to engagement service with activation and welcome call.
Step 2: Drive personalized, proactive care conversations across entire populations.
Step 3: Automatically trigger alert to care teams when an interaction identifies a patient or member who needs attention or intervention.
Step 4: Enable seamless, real-time connections to clinical services, resources, and support.
Step 5: Accelerate delivery of information and well-being data that leads to better health and lower costs.
Meet Angel: Award-Winning AI Voice Nurse Assistant
With Care Angel, payers and providers can achieve the following goals:
Contact 100% of members for care management and proactive health and SDoH engagement
Extend clinical capacity by 6X with check-ins at home for acute, episodic, or chronic conditions
Identify specific care needs and automatically target transfer to the appropriate resources to drive down clinical costs by 7.7X and improve population health.
Angel comes to life through a secure, HITRUST-certified platform that supports healthcare organizations’ HIPAA compliance. Launching hundreds of thousands of personalized interactions with members and patients, Angel reaches millions of at-risk patients. That’s for post-discharge, pre-post procedure follow-up care, medication adherence, management of chronic conditions such as diabetes and hypertension, or any clinical outcome or performance measure you’re striving to achieve.
Want to Learn More? Contact Care Angel Today!
To learn more about Care Angel, contact us today by calling 877-902-6435 or completing the form. We look forward to working with you and providing you with the health engagement and care management tools you need!